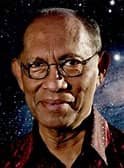
Hector Magno
Independent Computer Scientist, USA
Title: # Measuring the Benefits of Mass Vaccination Programs
Submitted Date: 30-08-2021
Biography
Hector Magno is a researcher, data analyst, and software developer. He attended UC Berkeley as a Regent and Chancellor’s Scholar and earned a degree in Computer Science. He also attended UC Berkeley as a National Science Foundation fellow, earned a graduate degree in Computer Science
Abstract
Introduction Since the late 1940s, mass vaccination programs in the USA have contributed to the significantly reduced morbidity and mortality of infectious diseases. To assist the evaluation of the benefits of mass vaccination programs, the number of individuals who would have su ered death or permanent disability in the USA, had mass vaccination never been implemented, was estimated for several infectious diseases. Materials & Methods The estimates accounted for mortality and morbidity trends observed for the infections prior to mass vaccination, adjustments of pre-vaccine estimates using data recorded after vaccine licensure, and the impact of advances in standard of living and health care (such as improved nutrition, sanitation, hygiene, and the treatment of disease). The estimates also considered populations with and without known factors leading to an elevated risk of permanent injury from infection. The estimates are based on data principally from reports of the CDC, complemented by reports from other federal entities such as the US Bureau of the Census and the US Public Health Service. Data recorded in scientific journals (e.g., JAMA, Pediatrics, JID, NEJM, and JCO) were used in cases when data from government sources were unavailable or incomplete. The estimates focused on the population <80 years of age because the life expectancy in the USA was 79 years Results Mass vaccination programs may prevent 20 million infections and 12,000 deaths and permanent disabilities annually among individuals <80 years of age. Individuals who have conditions or behaviors that would put them at higher risk of permanent injury from infectious diseases comprise 90% of all the estimated cases of prevented death and permanent disability. Although 9,000 of the estimated prevented deaths and disabilities were from liver cirrhosis and cancer, mass vaccination programs have not, at this point, shown empirical impacts on the prevalence of those conditions. The table below summarizes the results for the infections examined in this report. Mass vaccination programs targeting rotavirus, hepatitis A, influenza, meningococcal disease, and pneumococcal disease were each estimated to prevent fewer than 100 deaths among individuals <80 years of age.

Reginald Gorczynski
Institute of Medical Science, Department of Immunology and Surgery, University of Toronto, Toronto, ON M5S 3G3, Canada
Title: #Lack of validity in concepts driving development of SARS-CoV2 vaccines.
Submitted Date: 01-06-2022
Biography
Institute of Medical Science, Department of Immunology and Surgery, University of Toronto, Toronto, ON M5S 3G3, Canada
Abstract
We have discussed earlier that current approaches to vaccination assume without proof that: a. following immunization most individuals are at similar risk of disease. b. relevant host resistant mechanisms (innate and/or acquired immunity) have been identified, and can be targeted appropriately to boost resistance c. after vaccination, individuals within a population react immunologically in the same way in terms of protective antibodies and/or cell-mediated reactivity (one size fits all) with equivalent and minimal side effects; and d. vaccination dose and frequency of administration is invariant in the population. These assumptions have been applied to widespread delivery of vaccines for a number of infectious diseases, with effective control for many of those. However, a clear weakness of this approach is that it discounts the growing evidence for individual variability in risk, in immune responsiveness, and in response to different doses of vaccine. These issues came to the fore while tailoring individual approaches to cancer therapy, but are now becoming more concerning as we come to grips with novel emerging infections, as has been highlighted during the recent SARS-COV-2 pandemic. We discuss below in more detail how innate immunity is likely an important component of viral resistance, and that viral responses to the innate immune system can help explain mutagenesis of SARS-CoV2 virus in the host. We also suggest that the inattention to mucosal immunity as a major component of respiratory virus infection, with instead a focus on induction of systemic immunity for SARS-CoV2 through conventional intramuscular injection, is a major error, and may have led to a gross misrepresentation of current vaccine efficacy and utility. Finally, we recapitulate our previous discussions of a characteristic epidemiology of this infection as it developed in distinct areas throughout the globe over the past 3 years, which led us to conclude that this reflected globally dispersed fragmented viral laden dust clouds brought down haphazardly to ground by local meteorological conditions and defined by capricious scales of turbulence. The emergence of new clusters of varying sizes independent of popular movement is readily explained on this basis. This hypothesis is testable, and offers hope that ‘lead-time†for future pandemics may be gained by sampling microbial content in the high stratosphere.